INTERNSHIP ASSESSMENT:
Posted in department of GENERAL MEDICINE from 12/12/22 to 11/2/23.
UNIT duties—-First 15 days (12/12/22-26/12/22)
Last 16 days (27/1/23-11/2/23)
I would check the vitals of my patients and update SOAP notes Daily morning and used to attend morning rounds
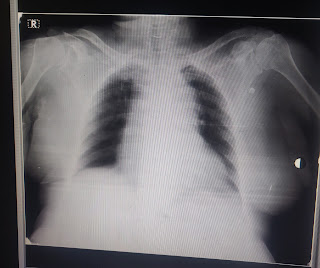
Have taken samples and took the patients for required investigations
Here are the blogs that I have done during my internship duties
https://sannithreddykasala.blogspot.com/2023/02/a-case-of-15-yr-old-male.html
https://sannithreddykasala.blogspot.com/2023/02/a-case-of-85-year-old-female.html
https://sannithreddykasala.blogspot.com/2023/02/a-case-of-70-year-old-frmale.html
https://sannithreddykasala.blogspot.com/2023/01/a-case-of-36-year-old.html
https://sannithreddykasala.blogspot.com/2022/12/a-case-of-55-year-old.html
https://sannithreddykasala.blogspot.com/2022/12/a-case-of-60-year-old.html
https://sannithreddykasala.blogspot.com/2022/12/case-of-68-year-old-female.html
During OP DAY
I took the basic history of the patients and wrote the investigation required under the guidance of PG
I have checked vitals of every patient
Examined for reflexes, postural hypotension, Romberg’s sign
Have learnt basic management protocol few common conditions like headaches, fever, chestpain
NEPHROLOGY DUTY:
Monitored Blood Pressures of the patients during dialysis and in the CKD ward.
while I was monitoring vitals , a patient had the Blood pressure-200/100 at 2:00AM.I've informed Dr.sailesh sir and he told to give Lasix and Nicardia,I got to know the role of lasix in CKD patients in clinical practice .
I encountered another patient with SOB at 2 am then I put him on nebulization with salbutamol and ipratropium bromide and checked it's bp it's was 180/110 then we NICARDIA 10 mg after nebulization his sob reduced and patient felt releif and next day morning dialysis was done
During ICU duty:
Monitored vitals of ICU and AMC patients.
Learnt drawing of ABG samples.
Inserted RYLES tube.
Done FOLEYS catheterisation .
Placed IV canula.
Assisted in Intubation with Dr Bharath and Dr shailesh sir
I've Learnt the role of atracurium in patients with high Respiratory Rate.
learned to connect the oxygen mask and the no: of litres of water to be adjusted based on requirement and CPAP.
WARD DUTY:
Monitored Bp for the patients with hypertensive urgency and made the chart of blood pressure recordings
Have attended the rounds.
Got SOAP notes updated of ward patients.
DURING PSYCHIATRY
Learned about importance of history taking and how history can guide us to probable diagnosis
vitals monitoring done for OP patients
Case related experience
1) Alcohol dependance- I've learnt the role of Loraz in alcohol withdrwal(1unit=30ml alcohol and we substitute 1 tablet of loraz for that) ,learnt the role of Baclofen in decreasing the cravings. Since thiamine is deficient in the we substitute that. I saw a patient who came early in morning with alcohol withdrawal tremors and he came drunk and want medication to stop drinking alcohol
2) Schizophrenia- I saw a 60 year male having delusion of infidelity, persecution, visual hallucinations. He was given Risperidone and Trihexyphenidyl(for side effect of Risperidone).
3) I've learnt how aggression(target oriented) is different from irritability(Generalized) for a person.
4) panic attack- Loraz is given for the patient.
5) I've learnt how we treat a patient with anger(uncontrolled anger, immediate- Haloperidol. Moderate anger- sodium valproate, mild anger -Loraz)
Learnt about audit score - a parameter used in evaluating alcohol dependence